In twenty-three years, we have experienced moments of joy and of relief. Likewise, we’ve known the terror that accompanied the dehydration and surgeries and the tumor on her skull. But sometimes there’s a quieter fear, a dread like a prickle on the scalp, often signaled by a beep in the night…
This past Thursday, Gabriella had been crabby. Nothing we did soothed her for long, and we were glad to get her into bed in the evening. When we attached her pulse oximeter to her toe, however, her heart rate was elevated. Then she had a seizure.
Gabriella has been experiencing seizures for years, but this one drove her heart rate to the highest level I can ever remember, nearly 170 (although not all of them come at night when we have the pulse oximeter attached). When she came out of it, Lisa took her temperature: no fever. But the pulse ox continued to beep, bringing that worry I’ve often known.
I have an ambivalent relationship with that device, with its white plastic wire and its digital display. It brings back awful memories of sleeping in hospital rooms during prolonged stays.
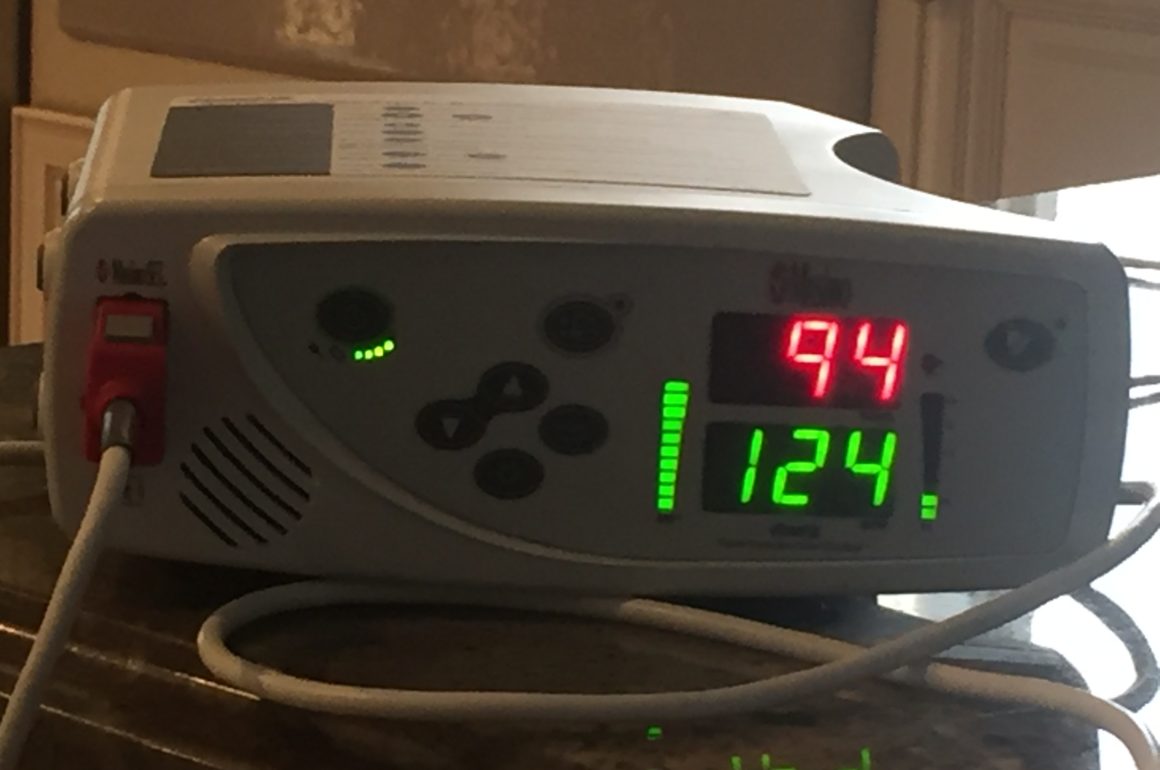
Even today, we use a baby monitor to track our daughter’s progress through the night. We hear the pulse ox beep when her oxygen dips below 90%, or when her heart rate exceeds 125 or goes under 50, which thankfully, is seldom. The sound it makes when alerted is insidious…beep-be-beep beep beep, beep-be-beep beep beep.
During the early years, it was unnerving to wake up to that clarion. I’d leap out of bed, hurry downstairs, wondering if my pulse was going as fast as hers. Upon reaching her room, the first thing I would do was to push the button to suppress the sound for the next two minutes. Sometimes the beeping was alerting us to something of concern. Just as frequently, it seemed, the small ring around her toe (it looks like an old-fashioned Band-Aid) has come loose or the connection skipped a beat. And when she sleeps, Gabriella’s heart rate often goes below 50. As a result, several times a week, I reset the lower limit to 45 to restore silence.
It can be easy to become complacent, and more so when you want it to be a mechanical failure or an excess of calm. But sometimes, it’s not so.
On Friday morning, her skin became warm. With her fever, she grew lethargic. We attached the pulse ox during the day, which was unusual, and found her heart rate peaking at over 150. The nurse listened to her lungs and said she thought they sounded junky. But if she was congested, why was her oxygen level so strong?
Lisa consulted Gabriella’s doctor and got a prescription for an antibiotic, plus we gave her Tylenol. I sat alongside the pulse oximeter, poking my thumb at the button every time it sounded, trying to get it before the first beep bloomed into that horrid sequence.
We alternated being on-call for two-hour increments. That night was stable, but I awoke at 7 a.m. to the beep-be-beep beep beep-ing. My first thought was that her heart rate had fallen once more under 50. But when I pressed my thumb to silence the pulse ox, I found that her oxygen level had dropped to 89, then 88. Most mornings, the beeping is enough to wake her, but she slept on. Her forehead was warm again, so I put a Tylenol caplet in a syringe with water to dilute it for delivery through her G-tube.
I waited in the shadows, leaning over to push the button every two minutes. The numbers became depressed: 86, 85, 83, 80, and down into the 70s. This was during my shift and I wanted to let Lisa catch up on rest, so I tried rewrapping the toe-ring and got immediate gratification, with the oxygen level soaring to 94. But it soon slipped back into the 80s and then to 75. I flipped her to her other side, but that didn’t help either.
I wondered if I would need to haul out the oxygen concentrator, a rolling piece of equipment that has always intimidated me, and not least because its use often heralds a trip to the hospital. But with first light, things normalized.
As the day progressed, we held our breath and wondered. Whether the fever would persist. Whether she would suffer more seizures. And whether more beeping in the night would bring another round of dread.
Saturday was much like Friday. In no particular order, Gabriella spiked a fever, we administered Tylenol and the antibiotic, she cooled down, she got an extra breathing treatment, her heart rate normalized. By bedtime, she seemed better.
Again, we traded off that night. When I woke for my shift, I heard a great rumbling. Gabriella’s oxygen had fallen and, after trying chest PT and flipping her from side to side, Lisa had set up the O2 concentrator. The growling-wheezing sound brought a new round of anxiety, but even that didn’t drown out the beeping.
Sunday was a lot like the prior two days. With three doses of the antibiotic down, Gabriella seemed to be better by bedtime, then things slipped again. This time we didn’t hesitate long before setting up the concentrator, facing another night of lousy, interrupted sleep. By Monday morning, she was cheerful, trying to encourage us despite a low-grade fever.
Once more the day held new promise. And yet I know that when darkness falls, I will feel that familiar dread, my subconscious mind alert. Awaiting those things that go beep in the night.